Back Pain Imaging
Adam Guttentag M.D.

Wasted time?
Radiology departments do lots of imagingfor low back pain.
X-rays, CT, MRI etc.
How much makes a difference?
Studies show advanced imaging in acuteback pain and sciatica doesn’t changeoutcomes, but improves diagnosticconfidence.

Causes of back pain and sciatica
Paraspinal musclesand ligaments
Synovial joints:
Facet and sacroiliacjoints
Disc disease
Tear of annulusfibrosis
Specific nerve rootimpingements
Spondylosis
Spinal stenosis
Foraminal stenosis
Bone disease
Tumor
Fracture
Infection
Epidural abscess
discitis

Acute Back Pain
2nd most common complaint to primarycare physician
>75% of adults will suffer it at some time.
90% will resolve without intervention (orimaging), most without a specific dx.
Among patients with sciatica, only <10%will need surgery.
Whom to image?

Back pain imaging—false positives
Most adults over 40 will have degenerativechanges on x-rays
MRI shows disc pathology in the majorityof adults
Many asymptomatic people have discbulges and protrusions.
So, imaging is likely to result in anabnormal report.
But correlation between radiographicfindings and clinical symptoms is poor.
When to image?


When to image in patients with acuteback pain?
Most authorities suggest conservativetreatment for 4-6 weeks unless there are“red flags”:
Look for historical and physical findings that raiseclinical question of infection, tumor, or seriousneurological impairment
Even positive findings of degenerative diseaselike disc extrusions and spinal stenosis are noturgent and will be treated conservatively at first.

“Red flags” for early imaging
Severe progressive neurological deficit
Fracture?
Major trauma or minor trauma in osteoporotic pt.
Tumor?
History of cancer, weight loss
Pain worse at night or when supine
Infection?
Recent bacterial infection, immune supression, fever,IVDA

Imaging options
Radiography
CT
Better for fine bone detail, arthritis
As good as MRI for acute disc disease
Myelography as adjunct
MRI
Very good for disc, paraspinal pathology, stenosis
Infection
Marrow disorders
Contrast for infection, post-op, tumor
Bone scan
Not for primary imaging in most cases
Diskography

Radiography
AP and lateral films
Oblique films
Flexion / extension films


Radiography
Diagnoses that can be made on AP andlateral:
Spondylolisthesis
Compression fracture
SI joint disease
Disc degeneration
Facet arthritis
Tumor
Infection in disc space



Discitis

Radiography
Diagnosis bestmade onoblique films:
Spondylolysis
Facet arthritis
Foraminalstenosis(cervical spine)


Facet joints

Radiography
Diagnosis made with flexion / extensionfilms:
instability



Spondylolysis
Stress fracture through pars interarticularis
If bilateral, can cause spondylolisthesis


spondylolosthesis
spondylolysis
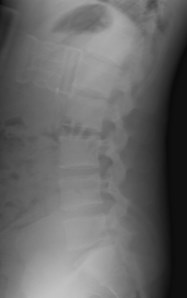
Sagittal reformatted CT

Cross Sectional Imaging: CT and MRIWhy?
Confirm extent of degenerative disease and spinalstenosis.
Search for confirmatory findings in patient with aspecific radiculopathy if surgery is contemplated.
Occult back pain not responding to conservativetreatment
Rule out tumor or infection in appropriate patients

MRI
IV contrast only in:
Suspected infection
Suspected tumor
Post-operative spine
Recurrent disc vs. scar tissue
Contraindications to MRI—CT is anacceptable substitute for disc and bonydisease, but poor for infection or intrathecaltumor.

Anatomy


T1
T2
Conusmedullaris
Caudaequina

Anatomy

Nucleuspulposis
Nerve rootin foramen
Facet joint
disc
Nerve rootin foramen
Ligamentumflavum

Disc disease
After age 40, most adults have at leastsome desiccation and loss of height oflumber discs:
Low signal on T2 images.
Posterior or diffuse bulges and protrusions arecommon.
Jelly-like nuclear material leaks out through tearin annular fibers.

Intervertebral disc anatomy
Annular fibers
Nucleuspulposis

T2

Glossary of disc pathology terms
Herniation: nonspecific term subject tomisinterpretation.
Not recommended.
Bulge: diffuse enlargement of disc area
Very common
Usually not clinically important
May contribute to spinal stenosis
Protrusion: nucleus pulposis pushes focallythrough fibers of annulus fibrosis
Base wider than apex
May focally impinge on nerve or thecal sac

Glossary of disc pathology terms
Extrusion: nucleus material pushes out beyondposterior longitudinal ligament but remains incontact with disc space
Apex wider than base
Likely to impinge on nerve roots
Sequestration: Disc fragment isolated from parentdisc

Glossary of disc pathology terms
Localizing terms:
Central
Paracentral
Foraminal
Lateral

Annular disc bulge
Disc bulges diffusely

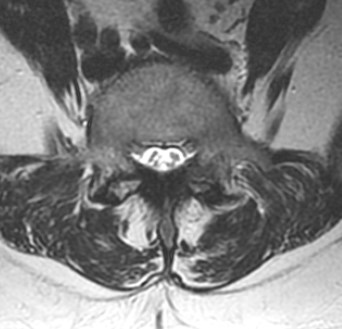
Broad based disc protrusion




Paramedian disc protrusion


Normal right L5 root
Displaced left L5 root
This should correlate with a leftL5 radiculopathy.

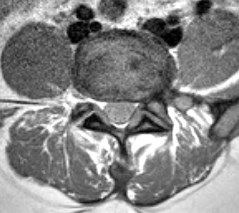
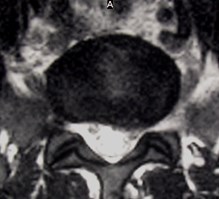
Disc Extrusion
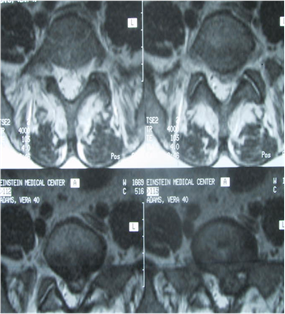
Axial T2

Sag T1
Sag T2

Foraminal Disc Extrusion

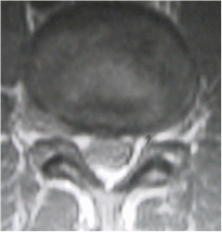
Foraminal Fat Obliterated
Normalforamina

Even large disc extrusions will resolvespontaneously



Several months later
Large extruded disc

Spondylosis
Degenerative disease
Disc dessication, bulges and protrusions
Ligamentum flavum hypertrophy
Facet arthritis and hypertrophy
Degenerative spondylolisthesis (seen in 7% of asxpatients)
Osteophyes
All combine to cause stenosis of spaces thatnerve roots pass through:
Canal, lateral recess, neural foramen

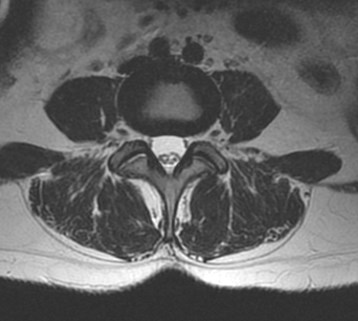
Spaces for nerve roots
Nerve root in lateral recess
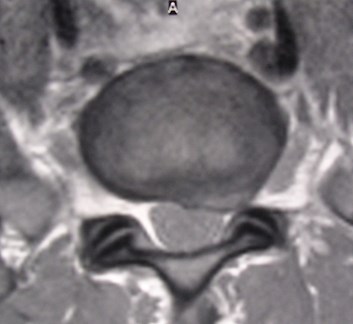
Neural foramen
Cauda equina roots in spinal canal

Facet joint arthritis


Spinal stenosis
Symptoms
Neurogenic claudication
Pain relieved with sitting, bending forward
Progressive pain
+/- radiculopathy, cauda equina syndrome
+/- low back pain
No specific measurement to define it in the lumberspine.
Many improved with nonsurgical therapy

Spinal stenosis
Contributing factors:
Disc bulges and protrusions
Facet arthropathy
Ligamentum flavum hypertrophy
Posterior vertebral body osteophytes
Anterior and lateral osteophyes generally notimportant
Spondylolisthesis
Not spondylolysis alone

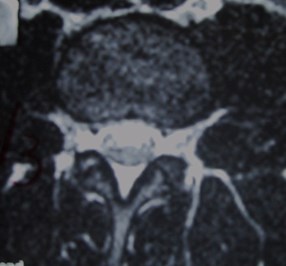
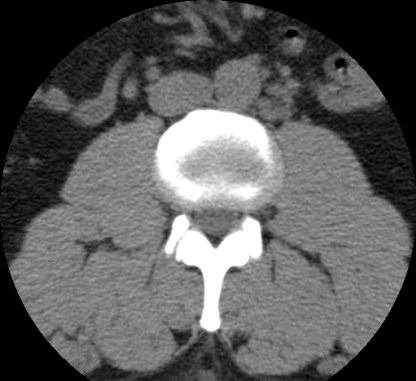
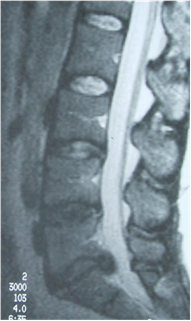
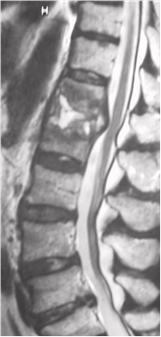
Spondylosis(Degenerative Disease)


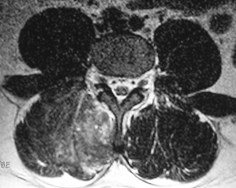
Sag T2
Axial T2
Axial CT
Annular disc bulge and facet arthropathy causespinal stenosis

Spondylosis causing spinal stenosis




What does that report mean?
Facet disease:
Common in older patients
May cause pain radiating to hip, simulating sciatica
Predisposes to dynamic instability
Contributes to spinal and foraminal stenosis
Mild disc bulges or protrusions
Very common incidental findings
Focal sciatica
Spinal stenosis only if large or in combination withother factors
Usually not significant unless good correlation withsx.

What does that report mean?
Look for key words and descriptions:
“spinal stenosis”, “foraminal stenosis”
Nerve root “displacement”, “compression” or“impingement”
Is a specific root involved?
Does it correlate with symptoms?

Spinal and Epidural Infection
High risk populations:
Immunocompromised
AIDS
Transplant
Chemotherapy
Endocarditis or sepsis
Postoperative patients especially with hardware
Tuberculosis: not necessarily immunecompromised

Bacterial discitis
T1 Sag
T1 Axial With GD

T2 Sag

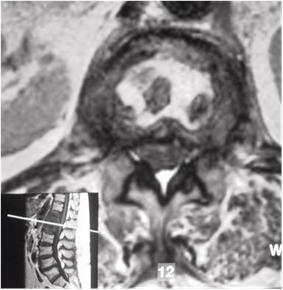
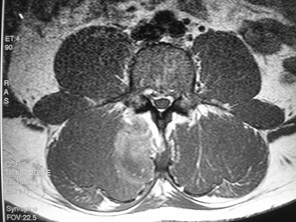
Tuberculous spondylitis withepidural abscess


T1 with Gd
T2
Enhancingvertebral body
Non-enhancingfluid in discspace andepidural space


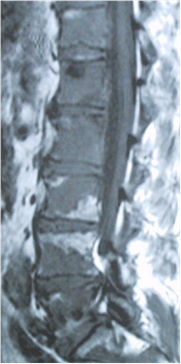
IV drug user– paraspinal abscess
T1 unenhanced
T1 enhanced
T2 unenhanced

Compression fracture:Benign or malignant?
Often diffucult to distinguish cause of acutecompression fracture
History of osteoporosis?
Osteoporosis may indicate multiple myeloma inpatient without risk factors.
History of primary tumor?
MRI good for survey of marrow at other levels tolook for other metastases
Bone scan may serve same function

Compression fracture:Acute or chronic?
Many patients have unsuspected oldcompression fractures:
Cheapest evaluation: check old films!
Bone scan can prove a fracture is old
May remain positive for up to two years
In elderly, may not be positive in first day
MRI can detect acute marrow edema

Compression Fracture—new or old?
•New
•Hypointense T1
•Hyperintense T2
Easily missed if only T2Sequence used
•Chronic
•Same marrow signalas other vertebralbodies on all pulsesequences


T1
T2

Metastatic disease
On T1 weighted images,discs should be darkerthan marrow tissue
Tumor brighter on T2weighted images,enhances with contrast
Exception—scleroticprostate metastases

Questions

All of the following contribute tospinal stenosis except:
Facet arthritis
Spondylolysis
Spondylolisthesis
Disc protrusion
Ligamentum flavum hypertrophy

Patients for whom early imaging isrecommended:
35 year old with AIDS and back pain
35 year old mother of three with sciatica
70 year old with breast cancer and severe newback pain
45 year old man with severe back pain aftermoving furniture
65 year old with saddle anesthesia

All statements are true except:
Disc protrusions commonly resolvespontaneously.
MRI can reliably identify the level of nerve rootinvolvement.
CT scanning is appropriate for evaluation ofsuspected spinal stenosis or disc pathology.
MRI is useful in distinguishing acute fromchronic compression fractures.

Reading
Brant-Zawadski MN et al Low Back Pain. What theclinician wants to know. Radiology 2000; 217:321-330.